In order to prepare residents for both the rigors of residency training and preparedness for practice or fellowship after residency, we have developed a comprehensive curriculum that starts day one. We provide the following structured didactics and activities in addition to the day-to-day teaching you receive from your faculty on each rotation.
During your first week of orientation, you will be exposed to an array of activities to help prepare you for day one.
The week culminates with intern BootCamp where interns from all programs will rotate through stations including: night-float survival, transitions of care, central line insertion, and more.
To prepare you for the types of illness and spectrum of acuity you will see and manage as an intern, the entire summer is dedicated to you. Every day at noon you will participate in a session designed you solidify the foundational knowledge of the most common and acute pathologies you will see.
In addition to learning about specific disease processes you will manage as an intern, there are a variety of skills needed to help you succeed in residency. Our Wardcraft Series includes a weekly workshop to help build foundational intern skills. Workshops include:
- Fielding Nursing Calls
- Navigating EMR
- Oral Presentations
- Note Writing
- Building Problem Lists
- Clinical Reasoning
- Procedural Competencies
Following our summer lecture series, we offer a weekly protected educational half-day. Residents are freed from clinical duties for a 3-hour block every week to participate in didactics. Our didactics are tailored to the level of the learner: we offer a separate half-day for interns and another for senior residents.
The typical format consists of 3 sessions:
- Session 1 – Team-based learning didactic
- Session 2 – Morning report-style case conference
- Session 3 – Rotating Curriculum: Board Review, Journal Club, Ethics, Wellness, Simulation, Jeopardy, QI, High-Value Cost-Conscious Care
Our traditional didactics are led by experts in ambulatory medicine, hospital medicine, and all of the medicine sub-specialties.
During the morning report (usually held at noon), residents will be led through a case with a faculty member. In a large group format, residents are taught key clinical reasoning skills and critical thinking, in addition to building knowledge about disease states.
Each week, resident and faculty participate in a case conference presented by our PGY3 residents. In these conference we explore what happens when things don't go as planned. We discuss cognitive dispositions (formerly cognitive biases), system factors, and evidence-based learning to improve care.
The Department of Medicine hosts weekly Grand Rounds where trainees and faculty come together to learn from experts in the field. Speakers are chosen from a combination of local and national experts.
At UCSF Fresno, our Internal Medicine residency program features a comprehensive simulation curriculum that plays an essential role in resident training. Utilizing our state-of-the-art simulation center, residents take part in a variety of high-yield, hands-on learning experiences that build clinical confidence and support high-quality patient care. Regularly scheduled sessions include realistic code blue scenarios, rapid response training, and advanced clinical reasoning cases—all conducted in a safe, structured, team-based environment. The curriculum also includes dedicated Point-of-Care Ultrasound (POCUS) training with standardized patients, giving residents realistic opportunities to refine their skills in image acquisition and interpretation. In addition, the curriculum emphasizes procedural competency, providing residents with guided practice and feedback on essential bedside procedures such as lumbar punctures, thoracentesis, paracentesis, and central line placement. This deliberate practice model ensures that residents graduate with both the knowledge and procedural comfort necessary for independent practice.
For nearly 15 years, we have provided 3 retreats for our residents to build teams, build skills, and enjoy time with your colleagues outside of the hospital.
- PGY1 Team-Building Retreat - Early in the intern year, we focus on teamwork, trust, and fun.
- PGY2 Resident As Teacher Retreat - We know the transition to a senior resident is one of the most challenging transitions in residency. This 2-day retreat near Yosemite gives you leadership and teaching skills that will carry on through all 3 years and beyond.
- PGY3 Life After Residency - Residents will benefit from financial planners, recruiting, and tools to help prepare for fellowship in this 2-day retreat on the coast.

Gaining an understanding of evidence-based medicine (EBM) and developing skills in literature searching and appraisal is fundamental to life-long learning in medicine. As part of our core curriculum, we present interns with the foundations of EBM and prepare them to lead our senior resident journal club.
Intern Evidence-Based Medicine Workshops
For over 15 years, we have taught the fundamental skills of EBM in our six-session workshop series. These interactive workshops utilize a team-based learning approach to understanding the medical literature. Based on the Users’ Guides to the Medical Literature, we cover topics such as PICO, therapy articles, assessing harm, diagnostics studies, and more.
Interns will learn to:
- Formulate clinical questions,
- Find the best relevant evidence,
- Appraise risk of bias of various study types,
- Assess the results,
- Generalize the results to their patients, and
- Engage patients in making a shared-decision.
Resident-Led Journal Club
During the PGY2 and PGY3 years, residents will lead their peers in an interactive journal club. Residents choose articles from a repository of the most influential articles of the prior year. Paired with a faculty mentor, the lead large group discussions of assessment and appraisal.
Our sessions follow a novel peer-reviewed format that incorporates principles of active learning and adult education. The process helps residents learn to draw their own conclusions from the study design and results that are independent of the author’s conclusions, fostering independent critical-thinking skills.
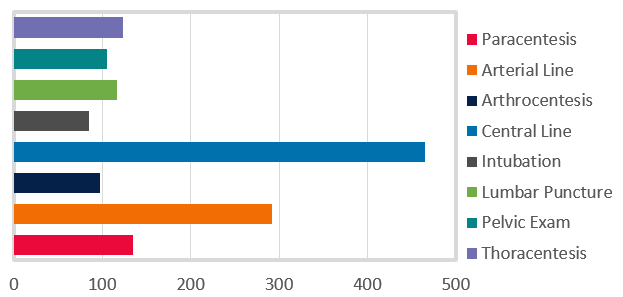
We provide an unparalleled opportunity to develop procedural competencies while in residency. Our graduates complete training with a broad set of procedural skills. All resident will become privileged in the following procedures:
- Central venous catheter insertion
- Arterial catheter insertion
- Lumbar puncture
- Thoracentesis
- Paracentesis
- Pelvic exam
In addition to our required procedural competencies, many residents develop competencies in endotracheal intubation, arthrocentesis, incision & drainage, and punch biopsies.
In just one academic year, our residents logged over 1400 procedures.
All interns will spend dedicated time in one of our state of the art simulation centers, training in ultrasound techniques and bedside procedures.
Additionally, residents will perform various procedures on their patients while rotating on our robust critical care and wards rotations.
While the number and variety of procedures that internists perform has dwindled elsewhere over the years, the strength of our procedural training has only grown. We ensure that all of our graduates have the confidence and competence to perform all of the common medicine bedside procedures.